🌞 Why Is My Baby Yellow? Understanding Newborn Jaundice

Health & Sciences | The Varrock Street Journal
Good morning, readers! If you’ve ever been around a newborn, you might’ve noticed something a little surprising—a yellow tint to their skin or eyes. Maybe you are like me, and have heard your parents talk about how you or your siblings were yellow as well! For many parents, it can be alarming. Leaving many people wondering... Is this normal?
The answer? In most cases—yes. This yellowing is called jaundice, and while it’s common in newborns, it’s also something healthcare providers take very seriously. So today, we’re diving into what causes jaundice, when it’s harmless, and when it can be a sign of a bigger issue.
🍼 What Is Newborn Jaundice?
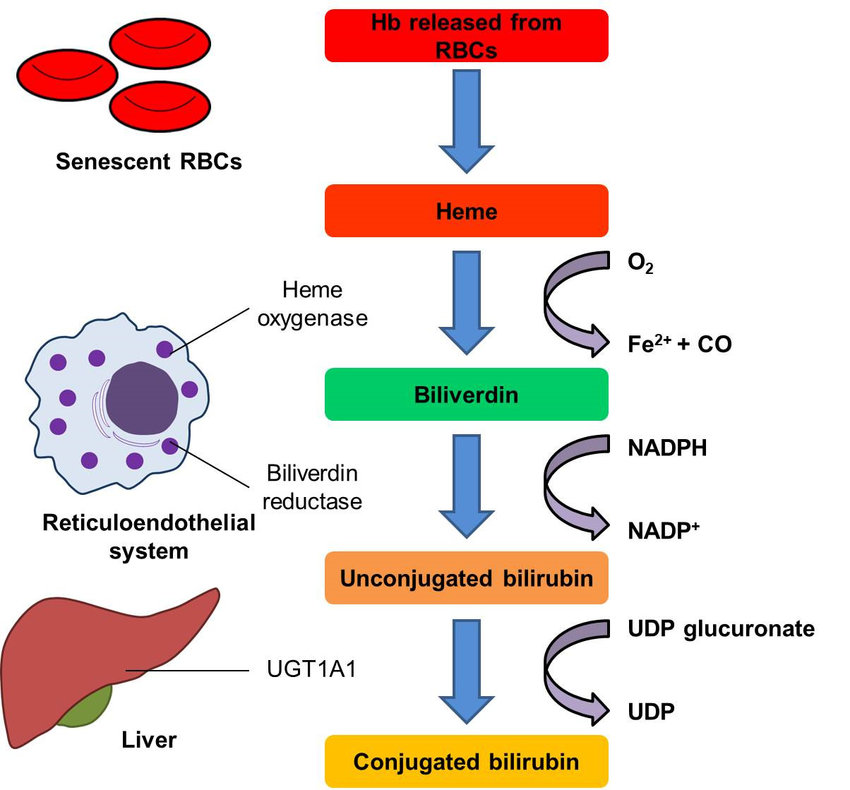
Newborn jaundice is a yellow discoloration of a baby’s skin and eyes caused by a buildup of bilirubin—a yellow pigment produced when red blood cells break down. Normally, the liver processes and removes bilirubin from the body. But in newborns, the liver isn’t fully mature, and sometimes it can’t clear the bilirubin fast enough.
As a result, over 60% of full-term infants and 80% of premature infants develop some level of jaundice within the first week of life.
🔍 Types and Causes
Not all jaundice is the same. Here are the key types:
- Physiological Jaundice (most common): Appears 2–4 days after birth and resolves within 1–2 weeks.
- Breastfeeding Jaundice: Occurs when a baby isn’t getting enough milk, usually in the first week.
- Breast Milk Jaundice: Starts after the first week and can last a month or more, but the baby continues to thrive.
- Pathological Jaundice: Appears within the first 24 hours or involves very high bilirubin levels—this requires immediate attention.
- Hemolytic Jaundice: Caused by blood type incompatibility (like Rh or ABO mismatch) leading to rapid red blood cell breakdown.
🧠 Why It Matters
While most cases of newborn jaundice are mild and resolve on their own, untreated severe jaundice can lead to serious complications, such as:
- Kernicterus – A rare but permanent type of brain damage caused by very high bilirubin levels.
- Hearing loss
- Cerebral palsy
- Developmental delays
That’s why early identification and monitoring are critical.
🩺 How Is It Diagnosed and Treated?
Diagnosis usually involves:
- Visual inspection (skin tone in natural light)
- Transcutaneous bilirubinometer (a non-invasive scan of the forehead)
- Blood test to measure total serum bilirubin (TSB)
Treatment depends on the level and cause of jaundice:
- ☀️ Phototherapy – The most common treatment. Babies are placed under special blue lights that help break down bilirubin in the skin.
- 💉 Exchange transfusion – Rarely used but necessary if bilirubin is dangerously high.
- 🤱 Feeding support – Encouraging frequent breastfeeding or supplementing to help flush bilirubin through stools and urine.
For mild cases, time and monitoring are often enough.
Here is a video to see what phototherapy for a newborn looks like!
🕰️ A Brief History
Before the 20th century, jaundice in infants was poorly understood and often fatal when severe. The development of phototherapy in the 1950s—discovered almost by accident by a British nurse—revolutionized care. Since then, global protocols have made it possible to treat jaundice safely and effectively around the world.
Yet in low-resource settings, access to care remains a challenge, and jaundice-related brain injury continues to occur.
🌍 Cultural Perspectives
In some cultures, jaundice is viewed as a natural rite of passage, while in others it may be associated with superstition or shame. This can delay seeking medical care. Education and community engagement are essential for early recognition and treatment.
Traditional remedies, such as herbal baths or sunbathing, may still be used—but not all are safe or effective. Culturally respectful care means integrating understanding with evidence-based practices.
🧪 Spotlight on the Future
Here’s what’s on the horizon:
- Home bilirubin monitors for at-risk newborns
- Smartphone apps for remote skin tone tracking in rural areas
- Artificial intelligence to predict which infants need treatment sooner
- Phototherapy blankets for low-resource settings
Innovation is helping us detect and treat jaundice faster, safer, and more globally than ever before.
😲 Did You Know?
- The word jaundice comes from the French word jaune, meaning “yellow.”
- Babies poop out bilirubin—so the more they feed and poop, the faster jaundice clears.
- Preterm infants have delayed liver maturity, making them more vulnerable to high bilirubin levels.
🧠 Reflection Questions
- Why do you think parents often underestimate jaundice at first?
- How can healthcare systems balance cultural sensitivity with timely treatment?
- What barriers still exist to treating jaundice in rural or underserved areas?
📚 References (APA Format)
American Academy of Pediatrics. (2022). Management of hyperbilirubinemia in the newborn infant 35 or more weeks of gestation. Pediatrics, 150(3). https://doi.org/10.1542/peds.2022-057994
Centers for Disease Control and Prevention. (2023). Newborn jaundice. https://www.cdc.gov/ncbddd/jaundice/index.html
Maisels, M. J., & McDonagh, A. F. (2008). Phototherapy for neonatal jaundice. New England Journal of Medicine, 358(9), 920-928. https://doi.org/10.1056/NEJMct0708376
Tsai, Ming-Tsun & Tarng, Der-Cherng. (2018). Beyond a Measure of Liver Function—Bilirubin Acts as a Potential Cardiovascular Protector in Chronic Kidney Disease Patients. International Journal of Molecular Sciences. 20. 117. 10.3390/ijms20010117.
👋 Final Thoughts
Newborn jaundice may be common, but it’s never something to ignore. With awareness, monitoring, and timely care, it can be managed safely—protecting babies from complications and giving families peace of mind.
📲 Let’s keep the conversation going:
- Instagram: @thevarrockstreetjournal
TikTok: @varrock.street.jo