💓 What’s That Sound? Understanding Heart Murmurs in Newborns and Children

Health & Sciences | The Varrock Street Journal
Happy Monday, Varrok Street Journal readers!
This week’s topic comes from a sound many healthcare professionals know well: the subtle “whoosh” that interrupts the rhythm of a beating heart. Known as a heart murmur, this sound can alarm parents when first discovered in a newborn or child. But here’s the good news—not all murmurs are a cause for concern.
Today, we’ll explore the types of heart murmurs, what causes them, how they’re detected, and what they can mean for your child’s health. Whether you’re a parent, a student, or just curious about how the heart works, this is one you won’t want to miss!
❤️ What Is a Heart Murmur?
A heart murmur is the sound of turbulent blood flow through the heart or nearby vessels, picked up during a physical exam using a stethoscope. It’s often described as a "whooshing" or "swishing" sound, and it can occur during systole (when the heart contracts) or diastole (when it relaxes).
Murmurs are not a diagnosis, but rather a finding. They can be innocent (harmless) or pathological (indicative of a heart problem).
👶 Types of Murmurs in Newborns and Children
1. Innocent (Physiologic) Murmurs
These are common and harmless, found in up to 50–70% of children at some point. The heart is normal, and the sound is due to blood flowing rapidly through a healthy heart.
✅ Key Features:
- Soft, low-pitched
- Changes with position (louder when lying down, softer when standing)
- No symptoms (child is active, growing normally)
🗣️ Common Innocent Murmurs:
- Still’s murmur: Musical or vibratory, heard best at the lower left sternal border
- Pulmonary flow murmur: Soft, blowing sound at the upper left sternal border
- Venous hum: Continuous sound heard over the neck veins, changes with head position
2. Pathologic Murmurs
These murmurs indicate a structural problem in the heart and require further evaluation by a cardiologist.
⚠️ Key Features:
- Louder (> Grade III/VI)
- Associated with other signs: cyanosis, poor feeding, shortness of breath, failure to thrive
- Doesn’t change with position
🫀 Common Pathologic Murmurs:
- Ventricular Septal Defect (VSD): Harsh holosystolic murmur heard at the lower left sternal border
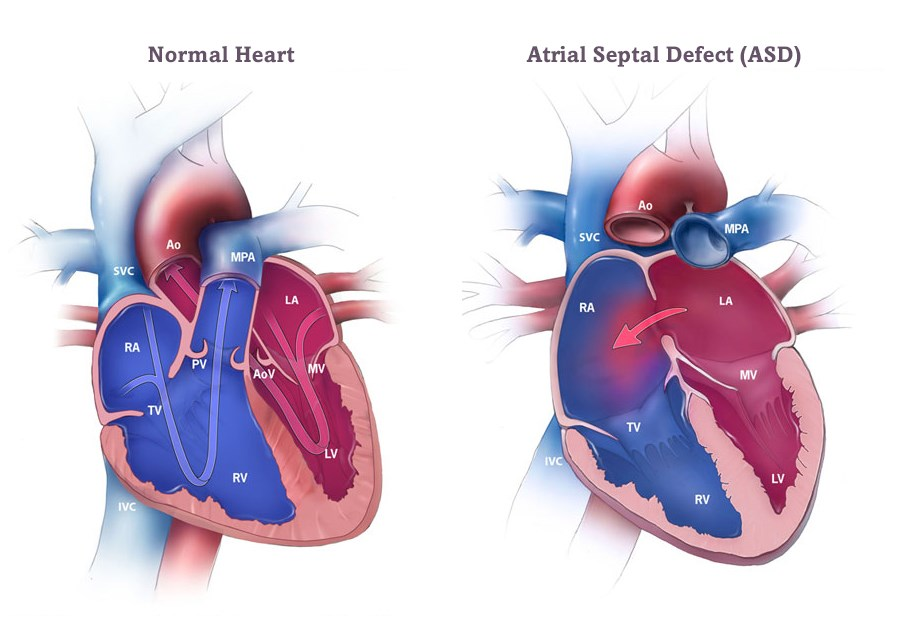
- Atrial Septal Defect (ASD): Systolic murmur with fixed split of S2
- Patent Ductus Arteriosus (PDA): Continuous "machine-like" murmur best heard under the left clavicle
- Tetralogy of Fallot: Harsh systolic murmur from pulmonary stenosis; may present with cyanosis
🩺 How Are Murmurs Evaluated?
When a murmur is detected, clinicians assess:
- Grade (I–VI): Indicates loudness
- Timing (systolic, diastolic, continuous)
- Location and radiation
- Changes with position
- Associated symptoms
If a murmur is suspicious, doctors may order:
- Echocardiogram (ECHO) – ultrasound of the heart
- Chest X-ray – to check heart size
- Electrocardiogram (EKG) – to evaluate rhythm
🧠 Why This Matters
For many parents, hearing that their baby has a heart murmur can be frightening. But the majority are innocent and resolve with age. Recognizing which murmurs need attention helps:
- Avoid unnecessary anxiety and testing
- Ensure early diagnosis of congenital heart disease
- Promote informed, compassionate pediatric care
🌟 Spotlight on the Future
Advancements in pediatric cardiology are making evaluations faster and more accurate:
- Portable handheld ultrasounds now allow point-of-care heart imaging in clinics
- AI-assisted auscultation tools are being developed to help doctors classify murmurs
- Genetic screening in newborns with pathologic murmurs is guiding personalized treatment for congenital heart defects
😲 Did You Know?
- The Still’s murmur, the most common innocent murmur, was named after Dr. George Frederic Still in the early 1900s.
- Many innocent murmurs disappear by age 7, but some persist into adolescence.
- Congenital heart defects are the most common birth defect—affecting 1 in 100 babies!
Here is a video discussing all types of murmurs if you would like to know more!
🧠 Reflection Questions
- Why might heart murmurs cause anxiety despite often being benign?
- What role could AI and digital stethoscopes play in rural or underserved areas?
- How can healthcare professionals better communicate the difference between innocent and pathologic murmurs to families?
👋 Final Thoughts
Whether it’s a quiet hum or a more urgent sound, heart murmurs are a message from the heart. Knowing how to interpret them helps ensure that every child gets the care they need—when they need it.
📚 References:
Adult Congenital Heart Association. (n.d.). Atrial septal defect. https://www.achaheart.org/your-heart/educational-qas/types-of-heart-defects/atrial-septal-defect/
American Heart Association. (2023). Heart murmurs in children. https://www.heart.org/en/health-topics/congenital-heart-defects/heart-murmurs-in-children
Mayo Clinic. (2024). Heart murmurs. https://www.mayoclinic.org/diseases-conditions/heart-murmurs/symptoms-causes/syc-20373171
Friedman, K. G., & Alexander, M. E. (2019). Approach to the pediatric heart murmur. New England Journal of Medicine, 380(3), 246-257.
📲 Stay informed and curious
- Instagram: @thevarrockstreetjournal
- TikTok: @varrock.street.jo