Tiny Tummies, Big Problems: Unpacking Pediatric Abdominal Conditions
Health & Sciences | The Varrock Street Journal
Good morning, Varrock Street Journal readers!
In the world of pediatrics, few things can be as alarming for parents—and as urgent for providers—as a baby or young child with sudden, severe abdominal symptoms. From projectile vomiting to a distended belly and bloody stools, abdominal conditions in children often require quick thinking, sharp diagnostic skills, and timely treatment.
Today, we’re exploring four major pediatric abdominal conditions you may hear about or encounter: pyloric stenosis, midgut volvulus, intussusception, and Hirschsprung disease. These conditions differ in cause and treatment, but all share one thing in common: they demand prompt attention.
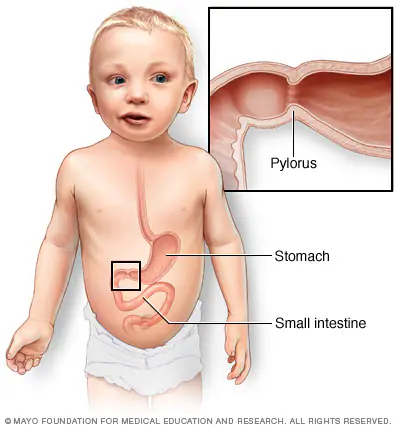
🍼 Pyloric Stenosis
What it is:
A condition where the pylorus (the muscular outlet of the stomach) becomes abnormally thickened, blocking food from passing into the small intestine.
Pathophysiology:
The muscle hypertrophies and narrows the gastric outlet, leading to obstruction and projectile, non-bilious vomiting in infants, typically between 2–8 weeks of age.
Risk factors:
- First-born males
- Family history
- Bottle feeding
- Exposure to macrolide antibiotics (like erythromycin) early in life
Diagnosis:
- Ultrasound: Gold standard—shows thickened pyloric muscle
- “Olive sign”: A firm, mobile mass in the right upper abdomen
- Electrolyte abnormalities: Hypochloremic, hypokalemic metabolic alkalosis
Treatment:
- Surgical pyloromyotomy (Ramstedt procedure)
- Rehydration and electrolyte correction pre-op
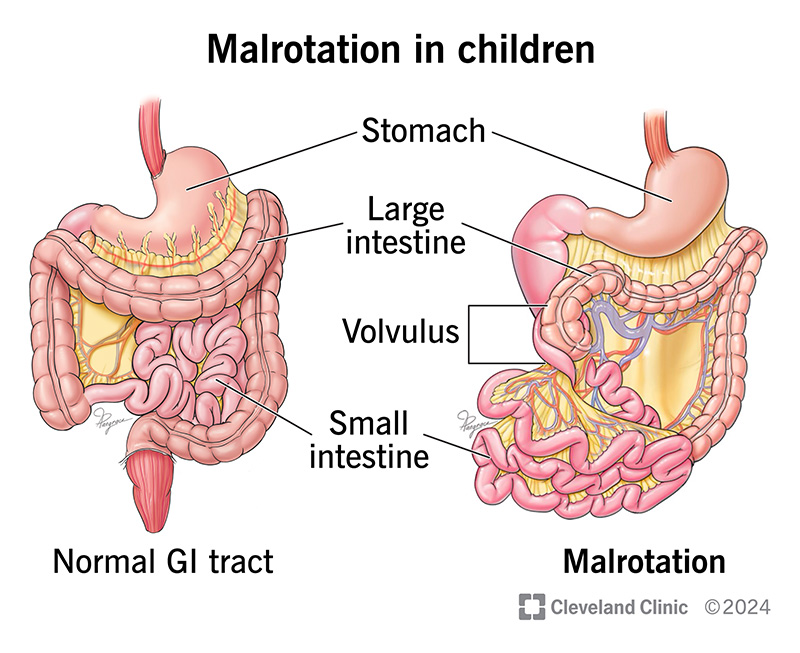
🌀 Midgut Volvulus (Malrotation with Volvulus)
What it is:
A twisting of the small intestine around its mesenteric attachment due to incomplete intestinal rotation during fetal development.
Pathophysiology:
This twist can cause bowel ischemia and necrosis by cutting off blood supply—it's a surgical emergency.
Risk factors:
- Congenital intestinal malrotation
- Newborns (most cases present in the first month)
Diagnosis:
- Upper GI series: Abnormal position of the ligament of Treitz; “corkscrew” appearance
- Can’t rely solely on physical exam—patients may present with bilious vomiting, abdominal pain, and distension
Treatment:
- Emergency surgery (Ladd procedure) to untwist and reposition the bowel
- Resection of necrotic segments if necessary
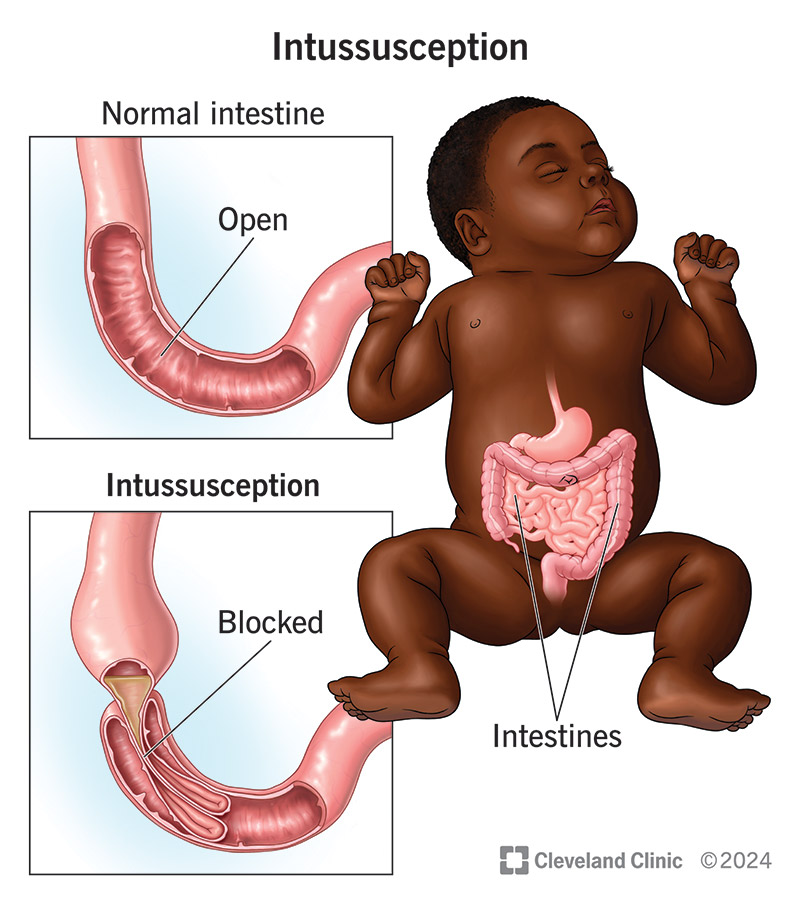
🧩 Intussusception
What it is:
Occurs when part of the intestine telescopes into an adjacent segment, leading to obstruction and reduced blood flow.
Pathophysiology:
Commonly involves the ileocecal region, and can be triggered by lymphoid tissue hypertrophy (e.g., after a viral illness). It’s the most common cause of intestinal obstruction in children aged 6 months to 3 years.
Risk factors:
- Recent viral infection (especially adenovirus)
- Meckel’s diverticulum
- Henoch-Schönlein purpura
- Cystic fibrosis
Diagnosis:
- Ultrasound: “Target” or “donut” sign
- History of intermittent abdominal pain, vomiting, “currant jelly” stools, and lethargy
Treatment:
- Air or contrast enema (both diagnostic and therapeutic)
- Surgery if enema fails or if signs of bowel perforation are present
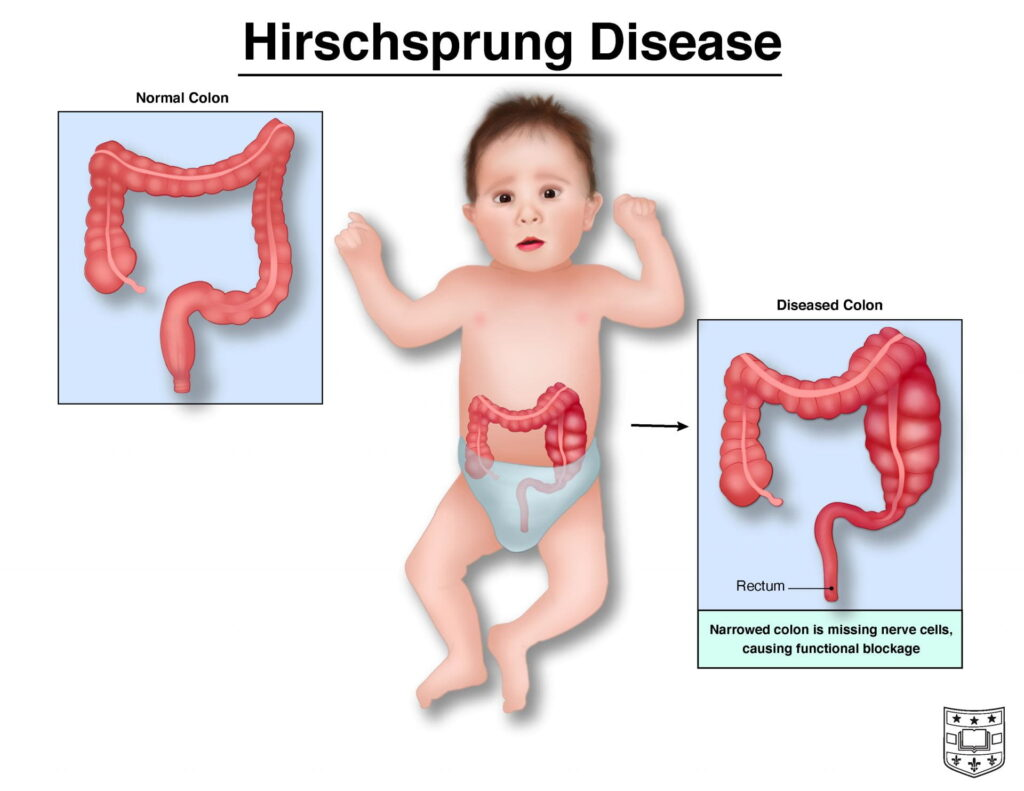
🚫 Hirschsprung Disease
What it is:
A congenital absence of enteric ganglion cells in the distal colon, resulting in a functional obstruction due to lack of motility.
Pathophysiology:
Without ganglion cells, the bowel cannot coordinate peristalsis, leading to chronic constipation, abdominal distension, and failure to pass meconium within 48 hours after birth.
Risk factors:
- Male sex
- Down syndrome
- Family history
Diagnosis:
- Rectal biopsy: Confirms absence of ganglion cells
- Contrast enema: Shows the transition zone between normal and affected bowel
Treatment:
- Surgical resection of the aganglionic segment (pull-through procedure)
- Ongoing management of bowel function and nutrition
🧠 Why This Matters
Recognizing signs of pediatric abdominal conditions early can mean the difference between routine treatment and life-threatening complications. Parents, teachers, and healthcare workers should be aware of warning signs like persistent vomiting, bloody stools, abdominal distension, and feeding intolerance. These conditions are rare but urgent, and when caught early, outcomes are excellent.
🌟 Spotlight on the Future
Advances in pediatric surgery and diagnostics are making care safer and faster:
- Miniaturized laparoscopic tools for less invasive surgery
- Faster bedside ultrasounds in emergency settings
- Genetic research into Hirschsprung and motility disorders
- Family education programs to improve early recognition and reduce ER delays
😲 Did You Know?
- Pyloric stenosis is 4 times more common in boys than girls
- Intussusception has a recurrence rate of up to 10% even after successful treatment
- Some babies with Hirschsprung disease only show symptoms months after birth, with severe constipation as the first clue
- Midgut volvulus can progress to bowel death in hours if untreated
🧠 Reflection Questions
- How can caregivers and healthcare providers improve early recognition of these pediatric emergencies?
- What role does family history play in guiding early screening or counseling?
- How can technology continue to support faster, safer care for infants and children?
👋 Final Thoughts
The tiniest patients often have the biggest challenges—but also the greatest recoveries. Awareness, quick action, and compassionate care go a long way in protecting the health of our youngest community members.
📚 References:
American Academy of Pediatrics. (2022). Common surgical conditions in infants. https://www.aap.org
Pumberger, W., & Zachariou, Z. (2018). Diagnosis and management of Hirschsprung’s disease in infants and children. World Journal of Gastroenterology, 24(47), 5435–5443. https://doi.org/10.3748/wjg.v24.i47.5435
Rothrock, S. G. (2020). Pediatric abdominal emergencies. Emergency Medicine Clinics of North America, 38(3), 563–583. https://doi.org/10.1016/j.emc.2020.03.005
📲 Join the conversation and keep learning:
- Instagram: @thevarrockstreetjournal
- TikTok: @varrock.street.jo