Inside the Mind: The Exams That Shape Psychiatry

It’s another beautiful Monday, Varrock Street Journal Community!
This week, we’re continuing our short psychiatry series in our weekly healthcare and medicine newsletter with an introduction to the Mini-Mental State Examination (MMSE) and the Mental Status Examination (MSE)—two critical tools used by psychiatrists and neurologists to assess cognitive function and mental health. Whether diagnosing dementia, evaluating psychiatric conditions, or monitoring recovery, these exams provide a structured approach to understanding a patient's mental state. But where did they come from, and how do they shape modern medicine? Let’s explore!
A Brief History of Mental Health Assessments
The concept of assessing mental function dates back centuries, but standardized tests only emerged in the 20th century. The MMSE, developed in 1975 by Dr. Marshall Folstein and colleagues, was designed as a quick, structured test to measure cognitive impairment, particularly in conditions like dementia. Meanwhile, the MSE has evolved as a broader, observational tool in psychiatry, assessing mood, thought processes, perception, and cognitive function.
These assessments have become integral in medical and psychiatric settings, offering a snapshot of a patient’s cognitive and psychological state.
What Are the MMSE and MSE?
Mini-Mental State Examination (MMSE)
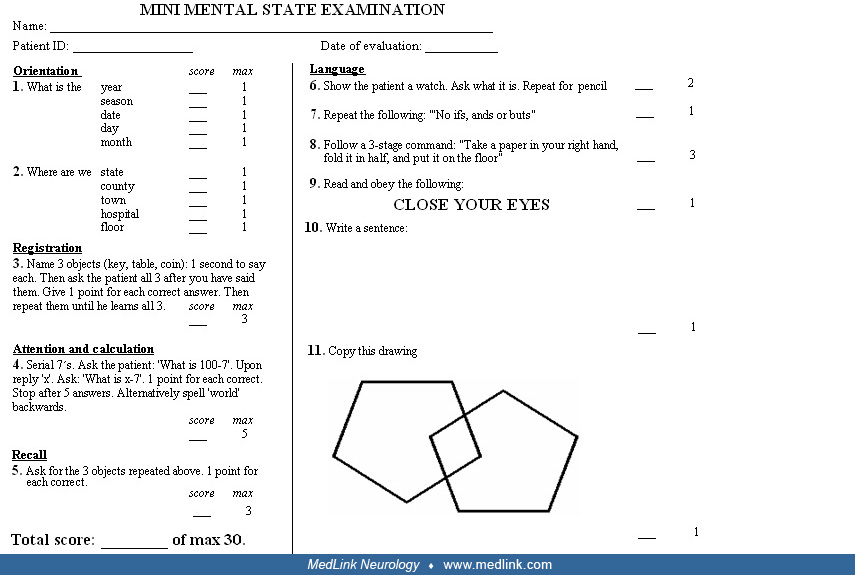
The MMSE is a 30-point cognitive screening tool used primarily to detect cognitive impairment. It assesses:
- Orientation (e.g., “What is today’s date?”)
- Registration (e.g., repeating three words)
- Attention & Calculation (e.g., counting backward by sevens)
- Recall (e.g., remembering the earlier words)
- Language & Praxis (e.g., naming objects, following commands)
A score below 24/30 suggests potential cognitive impairment, helping clinicians track conditions like Alzheimer’s disease.
Mental Status Examination (MSE)
Unlike the MMSE, the MSE is a comprehensive, subjective assessment performed by a clinician. It evaluates:
- Appearance & Behavior (e.g., hygiene, eye contact, agitation)
- Mood & Affect (e.g., happy, anxious, flat)
- Thought Process & Content (e.g., logical vs. disorganized thinking, presence of delusions)
- Perception (e.g., hallucinations)
- Cognition & Insight (e.g., memory, judgment, decision-making)
- Speech & Language (e.g., rate, tone, fluency)
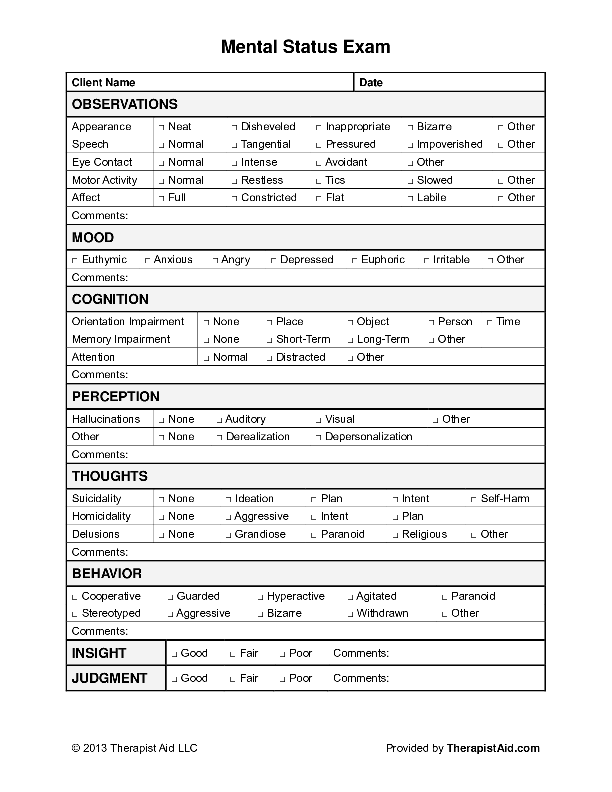
This structured evaluation is vital for diagnosing psychiatric conditions such as schizophrenia, bipolar disorder, and major depressive disorder.
Why These Exams Matter
Mental health assessments are essential tools for detecting neurocognitive disorders, psychiatric illnesses, and delirium in hospitalized patients. The MMSE offers an objective measure for tracking cognitive decline, while the MSE helps understand a patient’s thoughts, emotions, and behaviors in real-time. Together, they guide treatment decisions, determine the need for psychiatric intervention, and establish baselines for follow-up care.
How Are They Used in Hospitals?
Clinicians use these exams daily in neurology, psychiatry, and general medicine. Some examples include:
- Emergency Room: Distinguishing between psychiatric crises and delirium.
- ICU & Inpatient Wards: Assessing cognitive function after head trauma or infection.
- Geriatric Care: Diagnosing and tracking dementia progression.
- Psychiatric Units: Evaluating psychosis, depression, and suicidality.
Spotlight on Future Applications
While these tests remain widely used, research is exploring AI-driven cognitive assessments, digital mental health screening tools, and biomarkers for neuropsychiatric conditions. Newer models aim to refine cognitive testing, reducing bias and increasing accuracy for early detection of conditions like Alzheimer’s, schizophrenia, and depression.
Here is an example of a mini mental examination being conducted!
Personal Reflection
One unique aspect of psychiatric medicine is how different the treatment and evaluation of a patient is compared to other specialties. Most people are familiar with a doctor examining their eyes, ears, nose, throat, and abdomen, or listening to their heart. Of course, not every doctor follows this routine—an orthopedic surgeon evaluating a knee injury, for example, wouldn’t typically check your ears! However, psychiatry stands out even more because it is largely a hands-off specialty.
This approach serves several important purposes: it helps keep patients comfortable, fosters trust in the doctor-patient relationship, and reflects the collaborative nature of psychiatric care, which often involves a team of healthcare professionals working together to address a patient's mental and physical well-being.
Reflection Questions:
- How do standardized mental health assessments improve patient care?
- Should hospitals integrate AI-driven cognitive testing into routine care? Why or why not?
- How might early detection of cognitive impairment change treatment approaches in the future?
These assessments are powerful tools, helping clinicians diagnose, monitor, and treat cognitive and psychiatric conditions with precision. As technology evolves, so too will our approach to mental health assessment, ensuring patients receive the best possible care.
Thanks for reading! Stay curious, and see you next week for another deep dive into the world of science and medicine.
— The Varrock Street Journal Team