Gut Check: Understanding Diverticulitis and How to Keep Your Colon Healthy

Hello, Varrock Street Journal Community!
Building off of our discussion last week regarding colonoscopies and their role in preventing colorectal cancer (Read last week's newsletter here!), this week, we’re diving into an important and often misunderstood gastrointestinal condition: Diverticulitis and Diverticulosis. These conditions, affecting the colon, are increasingly common, especially in older adults. But what exactly causes them? How can they be prevented, and what treatment options are available? Let’s explore the key facts and latest research surrounding these conditions.
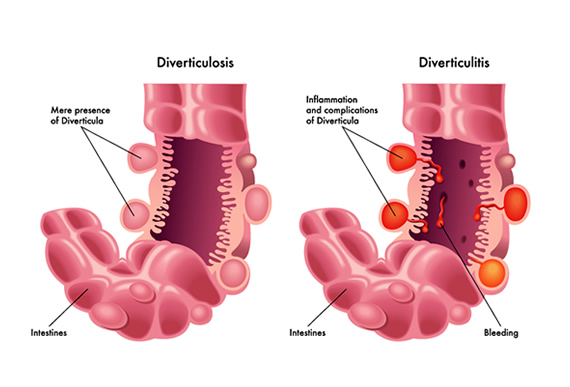
Understanding Diverticulosis and Diverticulitis
Diverticulosis refers to the formation of small pouches (diverticula) in the lining of the colon, which typically develop due to increased pressure within the colon. This condition is often asymptomatic, but complications can arise when these pouches become inflamed or infected, leading to diverticulitis.
Key Differences:
- Diverticulosis: Presence of diverticula without symptoms, often discovered incidentally during a colonoscopy.
- Diverticulitis: Inflammation or infection of diverticula, which can cause pain, fever, and digestive issues.
Risk Factors:
- Low-fiber diet leading to increased colon pressure.
- Aging, with prevalence rising in those over 50.
- Sedentary lifestyle and obesity.
- Chronic constipation.
(Reference: Strate LL, Morris AM. "Epidemiology, Pathophysiology, and Treatment of Diverticulitis." Gastroenterology. 2019.)
Complications and Treatment Approaches
While many cases of diverticulitis are mild and can be managed with rest and antibiotics, severe cases may lead to significant complications, including:
- Abscess Formation: Pockets of pus that may require drainage.
- Perforation of the Colon: A rupture in the intestinal wall that can lead to peritonitis, a serious infection requiring emergency surgery.
- Fistulas: Abnormal connections between the colon and other organs, such as the bladder, which may necessitate surgical correction. Read more here!
- Bowel Obstruction: Inflammation and scarring can lead to partial or complete blockage of the intestine, requiring intervention.
(Reference: Peery AF, Keku TO, Martin CF, et al. "Risk Factors for Diverticulitis in a Large Prospective Cohort Study." Am J Gastroenterol. 2016.)
Treatment Options:
- Mild Cases: Managed with oral antibiotics, a temporary liquid diet, and rest.
- Moderate to Severe Cases: Hospitalization may be needed for IV antibiotics, bowel rest, and possible surgical intervention.
- Surgical Treatment: In cases of recurrent severe diverticulitis or complications, procedures such as bowel resection may be necessary to remove the affected section of the colon.
(Reference: Hall JF, Hardiman KM, Lee SL, et al. "Colonic Diverticular Disease: Review of Current Guidelines and Future Directions." Clin Colon Rectal Surg. 2020.)
Why This Matters
Diverticulitis can range from mild discomfort to severe complications, including abscesses, perforations, and even life-threatening infections. Awareness and prevention strategies—such as maintaining a high-fiber diet and staying hydrated—can reduce risks significantly. Understanding the distinction between diverticulosis and diverticulitis helps individuals take proactive steps toward gastrointestinal health.
(Reference: Stollman NH, Raskin JB. "Diverticular Disease of the Colon." Lancet. 2004.)
Spotlight on Future Applications
Recent research is shaping new approaches for managing and preventing diverticular disease:
- Probiotics and Gut Health: Emerging studies suggest that probiotics may help maintain a healthy gut microbiome and prevent inflammation.
- Minimally Invasive Treatments: New techniques, such as endoscopic lavage and drainage, may help treat severe cases without the need for major surgery.
- Dietary Innovations: Fiber-rich, plant-based diets are being explored for their role in preventing diverticular disease and reducing flare-ups.
(Reference: Bolkenius K, van der Kaaij RT, Vennix S, et al. "Probiotics in the Prevention of Complicated Diverticular Disease: A Systematic Review." Int J Colorectal Dis. 2021.)
Reflection Questions
- How can dietary habits play a role in preventing diverticulitis?
- Should probiotics be a standard recommendation for individuals with diverticulosis?
- How can healthcare systems better educate aging populations on diverticular disease prevention?
- When should surgical intervention be considered for recurrent diverticulitis?
- What new treatments or approaches could improve outcomes for patients with severe complications?
This wraps up our weekly report! As always, we appreciate your engagement and insights. Let us know your thoughts in the comments or on social media.
See you next week!
- The Varrock Street Journal Team